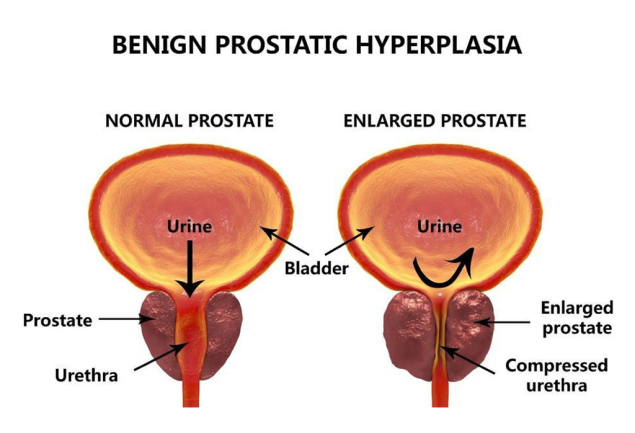

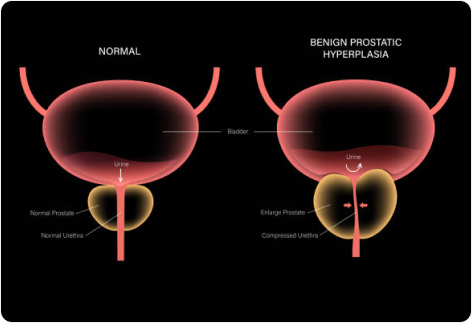
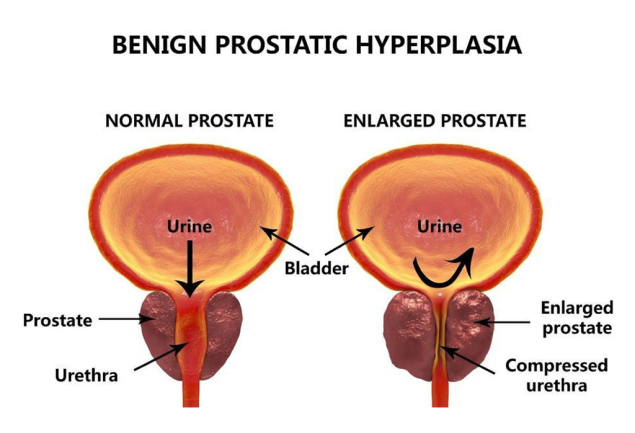
Benign prostatic hyperplasia (BPH) is a health issue which can become more common with age. We can also say that it is a medical condition men experience when their prostate is enlarged. Apart from that, it is also called benign prostatic hypertrophy or benign prostatic obstruction and is not cancerous in nature. To point out, the prostate is a small gland and its function is to make semen. It is placed or found below the bladder and often gets bigger as men get older. When the prostate is enlarged, it may give rise to certain symptoms which prove bothersome. The primary one is when the flow of urine from the bladder gets blocked. This also results in experiencing various kinds of complications related to the bladder, urinary tract or kidney. But, there are many treatment options available which can definitely help BPH patients. Perhaps discussing this matter with the right healthcare professionals is the wisest choice you can ever make. As a man ages, there are two main growth periods of the prostate. The first growth period occurs during puberty when the prostate doubles in size. In like manner, the second phase commences around the age of 25 and continues further for the rest of a man’s life. All things considered, benign prostatic hyperplasia usually occurs with the second growth phase. We shall try to encapsulate how this happens and affects the urinary tract system of an individual male. With the enlargement of the prostate, the gland presses and ultimately pinches the urethra. As a result, the bladder wall becomes thicker, which is also called bladder trabeculation. It weakens the bladder which loses its ability to empty completely and leaves some urine in it. Urinary retention and the narrowing of the urethra engender many problems associated with benign prostatic hyperplasia (BPH).
This indeed is one of the most classic questions that not only confronts the patients who suffer from BPH, but also the expert professionals. That’s because the actual cause or reason behind being affected with benign prostatic hyperplasia (BPH) is obscure. Older men are more prone to acquiring this medical condition than the younger ones. Some researchers are of the opinion that there could be some specific factors related to ageing and the testicles which may cause benign prostatic hyperplasia. As a matter of fact, men throughout their lives produce testosterone along with a female hormone called oestrogen. But as the men grow in age, the active testosterone levels in their blood decreases considerably, leaving behind a higher proportion of oestrogen. Empirical and measurable evidence based on principles of logic and reasoning, suggest that benign prostatic hyperplasia may be caused by presence of higher oestrogen levels within the prostate. The presence of oestrogen enhances the activity of the substances responsible for promoting prostate cell growth. Apart from that, there is another theory which principally focuses on dihydrotestosterone (DHT), a male hormone that plays a pivotal role in prostate growth or development. The research indicates that even after a drop in blood testosterone levels, older men keep on with producing and accumulating high levels of DHT in the prostate. Given these points, accretion of DHT could be a possible factor, further encouraging the prostate cells to grow continually. Surprisingly, scientists have also emphasised that men who do not produce DHT are less likely to develop benign prostatic hyperplasia. Changes in the balance of sex hormones as men get older could be another conceivable reason causing the prostate to get bigger. In the final analysis, it would suffice to say that there is a murky opinion behind all the veritable causes associated with benign prostate hyperplasia (BPH).
Some of the most prominent symptoms suggesting the existence of benign prostatic hyperplasia (BPH) may include the following:
Urination Frequency - An overactive bladder.
Urination Urgency - An inability in delaying urination.
Struggling in starting a urine stream.
An interrupted or weak urine stream.
Post micturition dribbling (PMD).
Nocturia- Getting up at night on a frequent basis to urinate.
Urinary Retention -The inability to empty all the urine from the bladder.
Urinary Incontinence- The accidental loss of urine.
Experiencing pain during urination or at the time of ejaculation.
Urine has an unusual smell or colour.
A healthcare professional diagnoses benign prostatic hyperplasia (BPH) on the basis of a personal, family medical history, a physical exam or a medical test. Taking note of a personal or family history is one of the first and foremost things a doctor may consider in order to diagnose BPH. Questions related to symptoms, history of recurrent UTIs, medications (prescribed & over the counter), the amount of liquid one takes in a day, whether he consumes caffeine or alcohol, general medical history, any major illness or surgeries are put forth. Besides that, he may conduct a physical examination by seeing if there is any discharge from the urethra and check for enlarged or tender lymph nodes in the groin or a swollen / tender scrotum. Performing a digital rectal exam which is a physical examination of the prostate is another viable option. It makes it easier to see if the prostate is enlarged, tender or has any kind of abnormalities requiring additional testing. On the other hand, a Urologist resorts to medical tests for diagnosing lower urinary tract issues related to benign prostatic hyperplasia. These medical tests may include urinalysis, a prostate-specific blood test (PSA), urodynamic tests, cystoscopy, transrectal ultrasound and biopsy. Talking briefly about these, there is a certain procedure that needs to be followed. When a urologist conducts urinalysis, a nurse or a technician would place a strip of chemically treated paper(dipstick) into the urine. Signs indicating the presence of infection in urine are noticeable if the patches on the dipstick change colour. Interpreting a PSA blood test can be hard as its ability to discriminate the nuances associated with cancer and prostate conditions such as BPH may not be perfect. In the same vein, the urodynamic tests focus primarily on the bladder’s ability to hold urine, along with emptying it uninterruptedly and completely. Cystoscopy is a method used for spotting blockage or stones in the urinary tract. This is done by inserting a tiny camera inside the urethra and passed into the bladder called a cystoscope. Likewise, a transcendental ultrasound requires a technician to insert a transducer into the man’s rectum, next to the prostate. The ultrasound images show the actual size of the prostate and presence of any abnormalities such as tumours. However, it cannot reliably diagnose prostate cancer. Lastly, biopsy comprises the procedure of removing a piece of tissue or collecting cell samples from a man’s body to be tested in a laboratory. This is usually done if a urologist identifies an area of concern when a man experiences symptoms appertaining to benign prostatic hyperplasia.
Treatment is an unavoidable thing when someone is suffering from benign prostate hyperplasia (BPH). After all, it lowers the risk of any further complications and helps a great deal on recouping good urinary tract health. Urinary retention and kidney damage are serious health related threats. It’s equally significant to realise that an enlarged prostate is not believed to enhance the risk of acquiring prostate cancer. However, treating benign prostate hyperplasia is indispensable. There are a lot of treatment options available and we shall try to elucidate them here.
Lifestyle Changes
Medications
Minimally invasive procedures
Surgery
The administrations of a healthcare professional in treating benign prostatic hyperplasia are based on the severity of symptoms a patient shows. That is to say, the way these symptoms affect a man’s daily life and his preferences are duly taken into consideration. There may be instances when men may not require treatment for a mildly enlarged prostate. In fact, resorting to the treatment options are only necessary when symptoms become bothersome, affecting the quality of life of an individual. A urologist may recommend regular check-ups instead of treatment in moderate cases. However, if he discovers that benign prostatic hyperplasia symptoms present a health risk and are bothersome, he often recommends treatment.
In case the BPH symptoms are mild or slightly bothersome, the first thing a health care provider would recommend is making some lifestyle changes. These may include lesser intake of liquids, caffeinated beverages and alcohol, monitoring the use of medications, training the bladder to hold urine for longer periods, exercising pelvic floor muscles and preventing or treating constipation.
A urologist may prescribe some medications which aid in stopping the growth or shrinking the prostate. These can reduce the symptoms associated with benign prostatic hyperplasia. To name a few, these include alpha blockers, phosphodiesterase, 5 alpha reductase inhibitors and combination medications.
Alpha blockers are FDA approved medications which help relax the smooth muscles of the prostate and bladder neck to reduce the bladder blockage and improve urine flow.
Phosphodiesterase - 5 inhibitors are prescribed by the urologists specifically for erectile dysfunction. They facilitate relaxing the smooth muscles in the lower urinary tract.
5-alpha reductase inhibitors aid block the production of DHT (dihydrotestosterone), a hormone that stimulates the development of male characteristics and accumulates in the prostate. DHT being present there, can cause prostate growth. These medications prevent progression of the prostate and can shrink it at the same time.
Combination medications is a combination of two or more drugs which may be administered in a single or a fixed dosage. These are believed to be more effective in improving symptoms, urinary flow and the overall quality of life. A urologist may prescribe a combination of alpha blockers and antimuscarinics for patients displaying overactive bladder symptoms.
There are a number of minimal invasive procedures developed by the researchers which succeed in relieving benign prostatic hyperplasia symptoms when medications fail to do so or prove ineffective altogether. These procedures destroy the enlarged prostate tissue or can widen the urethra, ultimately, relieving blockage and urinary retention caused by benign prostatic hyperplasia (BPH). Urologists use the transurethral method that refers to or involves inserting a catheter (thin flexible tube) or cystoscope through the urethra to reach the prostate. These procedures, although, may require administering local, regional or general anaesthesia. It’s equally imperative to know that destroying troublesome prostate tissues helps relieve many BPH symptoms; it however, doesn’t cure benign prostatic hyperplasia. A urologist may choose the right procedure after careful deliberations and examining the symptoms and overall health.
These include:
Transurethral needle ablation
Transurethral microwave thermotherapy
High-intensity focused ultrasound
Transurethral electro vaporisation
Water-induced thermotherapy
Prostatic stent insertion
For the long-term treatment of benign prostatic hyperplasia, a urologist would recommend removing the enlarged prostate tissue. In like manner, he may discuss or decide making cuts in the prostate for the purpose of widening the urethra. Some of the most common reasons why Urologists may recommend a surgery are:
When medications or minimally invasive procedures prove ineffective.
Patients experience extremely bothersome or severe symptoms.
When complications arise.
As has been noted, removing bothersome prostate tissue does relieve many benign prostatic hyperplasia symptoms, it does not cure the illness completely!
Surgery to remove enlarged prostate tissue includes:
Transurethral resection of the prostate (TURP)
Laser Surgery
Open Prostatectomy
Transurethral incision of the prostate (TUIP)
Except for an open prostatectomy, a urologist performs these surgeries using the transurethral method. Men who get surgical treatments, require local, regional, or general anaesthesia and need to stay in the hospital. Urologists also prescribe antibiotics before or soon after surgery to prevent infection. However, some urologists may prescribe antibiotics only after an infection occurs. A special catheter which is also known as Foley catheter, is inserted through an opening of the penis in order to drain the urine from the bladder into a drainage pouch after the surgery.
This surgical procedure involves cutting away a section of the prostate. A urologist inserts a resectoscope through the urethra to reach the prostate and cuts pieces of enlarged prostate tissue with the help of a wire loop. A special fluid then carries the tissue pieces into the bladder from where a urologist flushes them out when the procedure concludes. Not to mention, this is one of the most common surgeries and is considered as the gold standard for treating blockage of the urethra caused by benign prostatic hyperplasia.
An open prostatectomy surgery or radical prostatectomy is when a urologist makes an incision or cuts through the skin to reach the prostate. Another key point is that this surgery is usually conducted when the prostate is significantly enlarged, complications arise, or the bladder is damaged and needs to be repaired. Open prostatectomy requires general anaesthesia, and the patient may have to stay in the hospital for a longer period of time. The rehabilitation period is also likely to be a bit longer in this type of surgery. There are three types of open prostatectomy procedures, retropubic prostatectomy, suprapubic prostatectomy and perineal prostatectomy.
In laser surgery, urologists use a high-energy laser to melt away or vaporise the prostate tissue. A cystoscopy is used to pass a laser fibre through the urethra into the prostate. The laser destroys the enlarged prostate tissue or removes the excess tissue which was preventing the urine flow. However, laser surgery may not be a viable option when it comes to treating greatly enlarged prostates effectively.
TUIP is another surgical procedure used to treat benign prostatic hypertrophy (BPH). A urologist makes one or two small cuts in the bladder neck and prostate by inserting an instrument through the urethra. Consequently, it relieves the pressure resulting in improved urine flow. We can also call it transurethral incision of the prostate in other words. The rationale behind performing this surgery is to widen the urethra by making small cuts in the prostate and the bladder neck. According to some urologists, TUIP provides an equal amount of relief as does the TURP but with lesser risk of the side effects. After the surgery, the prostate, urethra along with the surrounding tissues might get irritated and swollen. This further may result in causing urinary retention.
Therefore, to prevent urinary retention, a urologist inserts a Foley catheter so that urine can be cleared out from the bladder. A Foley catheter has a balloon at the end that is inserted by the urologist into the bladder. After the insertion of the balloon inside the bladder, it is filled with sterile water to keep the catheter in place. Foley catheter generally remains in place for many days, but sometimes, might become a reason for recurring, painful, difficult-to-control bladder spasms the day after the surgery. Nevertheless, these spasms do not last long and eventually stop. A urologist may prescribe medications to relax the bladder muscles and to prevent recurring bladder spasms. However, patients undergoing minimally invasive procedures may not necessarily need a Foley catheter.